 Symbicort Vs Other Inhalers: Which Is Better?
Symbicort Vs Other Inhalers: Which Is Better?
How Symbicort Works Compared to Others 🔬
Symbicort combines a fast-acting bronchodilator with an inhaled steroid, delivering quick relief while reducing inflammation over time. Unlike single-agent rescue inhalers, it targets both immediate bronchospasm and chronic control in one device for many patients.
Formoterol’s rapid onset lets Symbicort be useful as both maintenance and reliever therapy, whereas some LABA partners act more slowly. This practical difference can improve symptom control and reduce exacerbations, something clinicians have definately noticed.
Compared to standalone inhaled steroids or short-acting relievers, combination inhalers simplify regimens and may boost adherence. But alternatives like LAMAs or high-dose ICS are preferable in certain patients with severe airflow limitation or frequent exacerbations.
Choosing between inhalers depends on goals, inhaler technique, and side-effect tolerance. Shared decision-making and objective measures like spirometry guide selection. Personal response varies, so follow-up and flexibility in therapy remain crucial to optimal long-term outcomes.
Real-world Effectiveness: Asthma and Copd Outcomes 📊

Clinical registries and observational studies often reveal how treatments perform outside trials. Patients report fewer exacerbations and emergency visits on combination inhalers like symbicort compared with bronchodilator-only therapy, though results vary by adherence and baseline severity. This real-world data is convincing yet nuanced, and benefits are not uniformly definately superior for every patient.
When clinicians look beyond randomized trials, patient technique, device familiarity, and comorbidities drive outcomes. Some cohorts show faster symptom relief and reduced steroid bursts with combination inhalers, while others show minimal advantage when adherence is low. Cost, education, and follow-up matter; noticable gains require ongoing support, individualized plans, and periodic reassessment so therapy achieve its full potential and frequent objective monitoring visits.
Side Effects and Long-term Safety Profiles ⚖️
When patients first try symbicort, they often notice quick relief but also experience throat irritation, hoarseness, or oral thrush; these are generally mild and manageable with rinsing after use. Less commonly, tremor, palpitations, or headaches can occur, and systemic steroid effects are rare at standard inhaled doses; physicians monitor growth in children and bone density in vulnerable adults.
Over months and years the benefits usually outweigh risks, yet monitoring remains important: vaccine status, adrenal suppression signals, and metabolic changes should be checked in long-term users. Adverse events may be underreported in trials, and real-world data show rare but serious exacerbations can occassionally appear, so shared decision-making and regular reviews help balance safety and control carefully.
Inhaler Devices, Technique and Patient Preference 💨

Patients often tell stories about devices — it's a small daily ritual: a press, an inhale, a breath held. Choice of device matters; metered-dose inhalers deliver drug fast but need coordination, dry powder inhalers demand a strong inspiratory effort, and breath-actuated systems reduce errors. Learning technique with symbicort or alternatives changes outcomes. Clinicians should watch technique, give personalized coaching, and use spacers or training aids when coordination is a challenge.
Preference hinges on lifestyle, dexterity, and confidence: busy commuters may favour handheld inhalers, whereas caregivers often prefer nebulisers for ease. Shared decision-making improves adherence; trials of devices let patients compare taste, sensation, and perceived relief. Follow-up must include technique checks and objective measures like peak flow. Cost, device availablity, and a patient's ability to aquire replacements also shape choice. Definately, the best inhaler is the one the patient will use correctly.
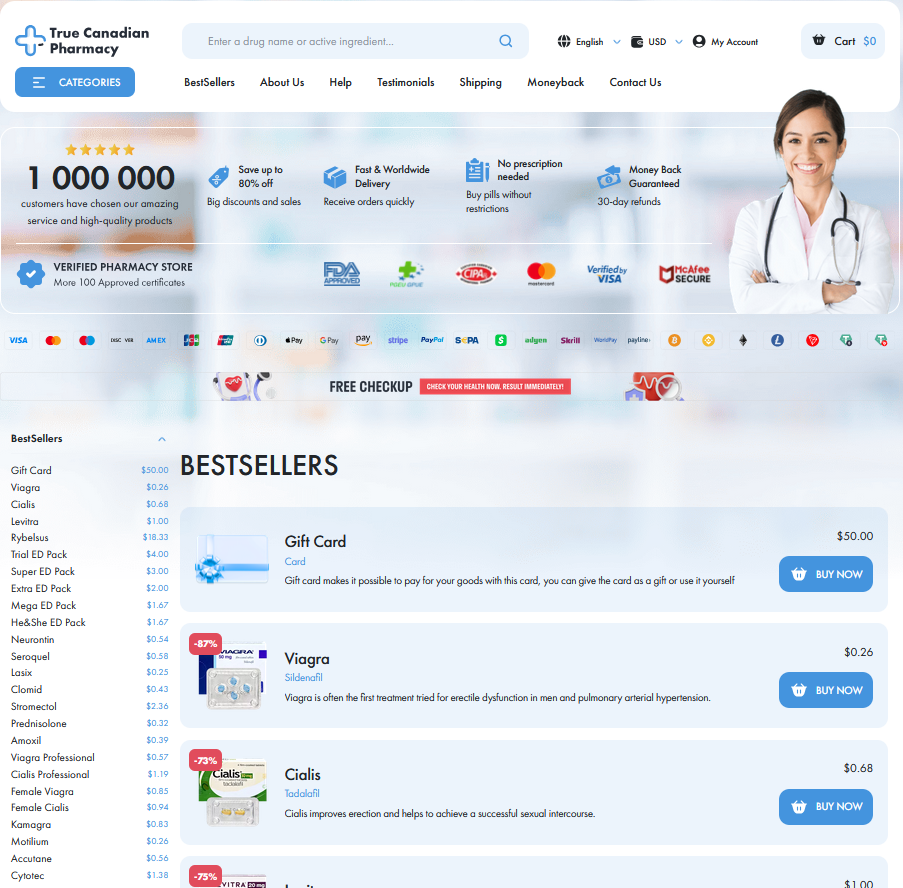
Cost, Insurance Coverage and Access Issues 💸
A trip to the pharmacy can feel like a small drama: prices vary wildly and choices bewilder patients who rely on daily inhalers.
For many, a branded product such as symbicort is effective, but co-pays, formularies and prior authorization create barriers that delay therapy. Mindful prescribing and competitive pricing programs can reduce out of pocket burdens for families.
Patient assistance programs and generic alternatives can help, yet paperwork and inconsistent coverage from year to year force difficult choices. Timing matters: early access helps.
Clinicians should discuss affordability openly, monitor refill patterns and refer patients to pharmacy counselors or social workers who can navigate coverage and Acommodate needs. Policy reforms and transparency would benefit patients nationwide.
Personalized Choice: Tailoring Therapy to Patients 🎯
Choosing therapy feels like matching a key to a lock: clinicians weigh severity, exacerbation history, comorbidities and inhaler skill to find the best fit. Some patients need rapid bronchodilation plus steroid control; others prefer simpler monotherapy. Clinicians must definately balance benefit, safety and adherence.
Phenotype, eosinophils, smoking status, comorbidities and cost guide individualized plans; regular review and inhaler training improve outcomes. Shared decision making respects preferences and risk tolerance while providing safety nets for exacerbations. Monitoring side effects and affordability ensures treatment is sustainable over time frequently. FDA label MedlinePlus
